Low-lying placenta (placenta praevia)
What is the placenta?
The placenta is the organ that helps your baby grow and develop. It’s attached to the lining of the womb and is connected to your baby by the umbilical cord.
The placenta passes oxygen, nutrients and antibodies (proteins produced by the immune system to protect your body from foreign objects, like viruses) from your blood supply to your baby.
It also carries waste products from your baby to your blood supply, so your body can get rid of them.
The placenta is usually delivered soon after your baby is born.
What are low-lying placenta and placenta praevia?
The placenta develops in the first few weeks of pregnancy, wherever the fertilised egg embeds itself in the lining of the womb. This could be along the top, sides, front or back wall of the womb.
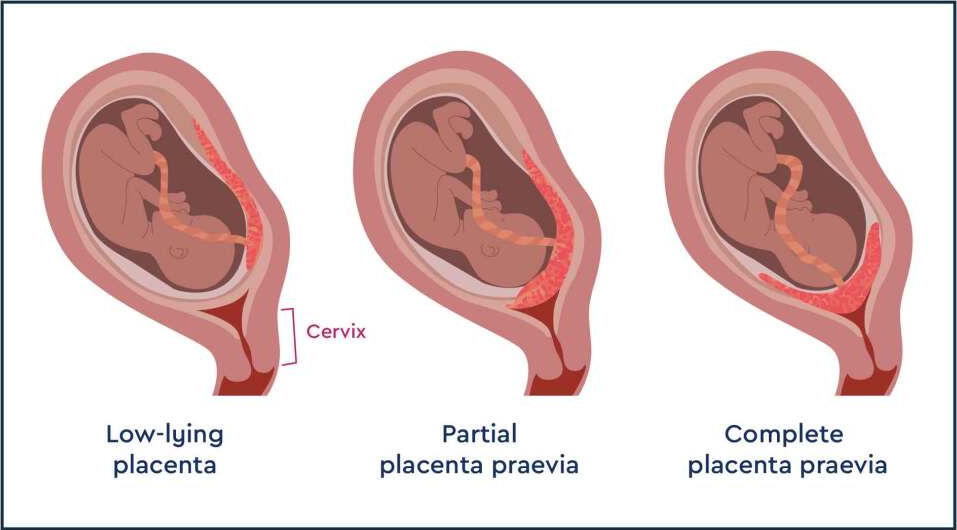
In most pregnancies the placenta attaches to the sides or top of the womb. However, for some women and birthing people, the placenta attaches lower down and may cover some or all of the inside of the cervix (entrance to the womb).
In most cases (9 out of 10), as the womb expands the placenta ends up being up and out of the way of the cervix.
- If the edge of the placenta is less than 2cm from the cervix, it is known as a low-lying placenta.
- If the placenta completely covers the cervix, it is known as placenta praevia.
Having a low-lying placenta does not cause pain in pregnancy.
A low-lying placenta can be posterior, which means that the placenta is towards your back and low. It can also be anterior, which means towards your front and low.
Are low-lying placenta or placenta praevia common?
Having a low-lying placenta at 20 weeks is not uncommon but in most cases this resolves itself and 9 out of 10 people who have a low-lying placenta at 20 weeks will not go on to have a low-lying placenta or placenta praevia later in the pregnancy.
Only 1 in every 200 people will still have a low-lying placenta or placenta praevia at the end of their pregnancy.
If you have had a baby by caesarean section (c-section) before, the placenta is less likely to stay in the lower part of the womb.
Who is at risk of placenta praevia?
Placenta praevia is more likely if you:
- smoke cigarettes or use cocaine
- have had fertility treatment to get pregnant, such as in vitro fertilisation (IVF)
- have had 1 or more caesarean sections
- have had previous miscarriage or abortions
- are aged 40 or older.
Can placenta praevia be prevented?
There is no one thing you can do to prevent placenta praevia. Although the factors above are linked to placenta praevia they haven’t been shown to be causes. Many of them are also beyond your control, your age for example.
If you smoke or use cocaine however it is best to quit as they affect your pregnancy health in many other ways
Does a low-lying placenta mean that my baby is a boy?
Research does show that placenta praevia is more likely in pregnancies where the baby is a boy. This doesn’t mean your baby will definitely be a boy but it does seem to be a bit more likely. Doctors do not know why this would be the case. The research does not cover the more common low-lying placenta, so this relates only to those who go on to have placenta praevia.
Is there anything I can do to help the placenta move up?
The placenta itself does not move once it has embedded at the beginning of pregnancy. It usually ends up being further up as the womb expands but it does not move itself and nothing can be done to make it move.
You are likely to need extra scans, so make sure you go to all your antenatal appointments and follow your healthcare team’s advice.
Talk to your healthcare team if you are having trouble attending your appointments for any reason. They may be able to make some adjustments.
How can a low-lying placenta or placenta praevia affect me and my baby?
Vaginal bleeding
If you still have a low-lying placenta or placenta praevia after 32 weeks, there is a risk that you may have vaginal bleeding. Bleeding from placenta praevia typically happens after sex or towards the end of your pregnancy and may be very heavy .
Preterm birth
There is also a chance your baby could be born prematurely (before 37 weeks) if you have placenta praevia or low-lying placenta.
Caesarean section
If the edge of your placenta is very close (less than 2cm) to your cervix (entrance to the womb), the safest way to give birth is by caesarean section. You can read more about this below.
Can I have sex with low-lying placenta or placenta praevia?
Sex may cause bleeding in women and birthing people with a low-lying placenta or placenta praevia after 20 weeks and your doctor or midwife may recommend that you avoid penetrative sex for that reason. In some cases placenta praevia is first discovered due to bleeding after sexual intercourse.
Your situation may depend on where the placenta is situated however, speak to your doctor about to be sure.
Read more about safety of sex in pregnancy with placenta praevia here.
Symptoms of a low-lying placenta or placenta praevia
Placenta praevia is usually spotted in the mid pregnancy ultrasound scan (18-21 weeks)
If your placenta is low at that scan, you'll be offered an extra scan later in your pregnancy (usually at about 32 weeks) to check it again.
Your midwife or doctor may think you have placenta praevia if:
- you have bleeding during the second or third trimester – it is likely to be painless and may happen after sex
- if the baby is lying in an unusual position, for example bottom first (breech) or lying across the womb (transverse).
If you have any bleeding during pregnancy, with or without pain, you should always get it checked out straight away. If you’re in your first trimester, contact your doctor, midwife or Early Pregnancy Unit. If you are more than 12 weeks pregnant, go to your local A&E or contact your hospital maternity unit immediately.
You may be advised to avoid having sex (including the use of penetrative sex toys) for the rest of your pregnancy.
What treatment will I have for placenta praevia?
Extra scans
If your placenta is low-lying at your 18-20-week scan, you’ll be offered another scan at around 32 weeks. This may include a transvaginal ultrasound scan, which is when a probe is gently placed inside the vagina to check exactly where your placenta is lying.
This is safe for you and your baby.
The length of your cervix may also be measured at your 32-week scan to see whether you may go into labour early and whether you are at increased risk of bleeding.
If the placenta is still low-lying at 32 weeks, you should be offered another ultrasound scan at 36 weeks.
The results of this scan will help you and your doctor plan the safest way for you to give birth. The level of monitoring you have will depend on your individual circumstance.
Medication
If you have placenta praevia, there is a higher chance that you may give birth prematurely. You may be offered a course of steroid injections between 34 and 36 weeks of pregnancy to help your baby’s lungs to become more mature. This can reduce the risk of your baby having serious complications.
If you do go into labour early, you may be offered medication to try to stop your contractions temporarily. This will give you time to have a course of steroid injections.
What precautions should I take if I have a low-lying placenta or placenta praevia?
If you know you have a low-lying placenta or placenta praevia, you should contact the hospital immediately if you have:
- vaginal bleeding, including spotting
- contractions
- pain, including any vague, period-like aches.
If you have any bleeding, your doctor may need to do an internal examination to check where it’s coming from. This is safe and they will ask for your permission before they start.
You may need to be admitted to hospital if you have vaginal bleeding. This is because there is a small risk that you could bleed suddenly and heavily. If this happens, you may need an emergency caesarean section.
In the second half of your pregnancy, have a hospital bag ready in case you need to go into hospital unexpectedly.
Anaemia
Anaemia is a blood condition that develops when you don’t have enough red blood cells. Red blood cells contain haemoglobin, a protein that carries oxygen around your body and to your baby.
If you have a low-lying placenta or placenta praevia, it’s important to try to avoid developing anaemia, which can be common in pregnancy. Eating a healthy, balanced diet can help you either prevent or manage anaemia. Iron supplements may also help if your healthcare team recommends them.
Your healthcare team will regularly check your haemoglobin levels throughout pregnancy. Find out about anaemia in pregnancy.
Giving birth with placenta praevia or a low-lying placenta
Your healthcare team will talk to you about what your options are for giving birth if your placenta is still low after 32 weeks.
You may be advised to give birth early if you have any heavy bleeding before your due date.
If the edge of your placenta is very close (less than 2cm) to your cervix (entrance to the womb), the safest way to give birth is by caesarean section.
This is because the placenta is blocking the birth canal or to avoid heavy bleeding during the birth.
A caesarean section may be recommended between 36 and 37 weeks, but if you have had vaginal bleeding during your pregnancy you may be advised to have your caesarean earlier than this.
If the placenta is further than 2cm from your cervix, you may be able to have a vaginal birth if you want one.
If you are having a caesarean section, a senior obstetrician (a doctor who specialises in pregnancy) will be there. This is because there is a risk of heavy bleeding during the surgery. If this happens, you may need a blood transfusion. This is more likely if you have placenta praevia rather than a low-lying placenta.
Let your healthcare team know as soon as possible if you do not want a blood transfusion.
Complications can be more common in caesarean sections if you have a low-lying placenta or placenta praevia.
Your doctor should talk to you about the risks of bleeding and hysterectomy (removal of the womb to help control heavy bleeding) before your caesarean. For most women and birthing people, the risk of hysterectomy is low and will only occur as a last resort if other measures to control bleeding don’t work.
Can I fly with low-lying placenta or placenta praevia?
If you have a low-lying placenta or placenta praevia you may be advised not to fly because of the risks of bleeding or going into labour before your due date. Check with your midwife or consultant if you are not sure.
Does a low-lying placenta or placenta praevia increase my risk of miscarriage?
Having placenta praevia increases the risk of premature birth rather than miscarriage. There is no evidence that the risk of miscarriage is increased with a low-lying placenta.
Your mental wellbeing
Finding out you have a complication in pregnancy can be hard. Having to be aware of certain symptoms, such as bleeding, or needing extra appointments and check-ups can be worrying and stressful. It may also be a lonely experience when those around you don’t understand what it’s like.
Remember that you can tell your midwife or doctor how you feel. They will do their best to reassure you and answer any questions you may have.
You can also call our pregnancy line on 0800 014 7800 (Monday to Friday, 9am to 5pm), or email us at [email protected].
If you are struggling to cope, there is professional support available. Talk to your midwife or GP about how you are feeling and they can help you access the right kind of support.
Find out more about looking after your mental health in pregnancy.
Royal College of Obstetricians & Gynaecologists (2018) Placenta praevia, placenta accreta and vasa praevia https://www.rcog.org.uk/en/patients/patient-leaflets/a-low-lying-placenta-after-20-weeks-placenta-praevia/
NHS Choices. The stages of labour and birth https://www.nhs.uk/pregnancy/labour-and-birth/what-happens/the-stages-of-labour-and-birth/ (Page last reviewed: 02/05/2023 Next review due: 02/05/2026)
Jenabi E, Salimi Z, et al (2022) The risk factors associated with placental previa: an umbrella review. Placenta Jan:117:21-27 doi.org/10.1016/j.placenta.2021.10.009.
Faiz AS, Ananth CV (2003) Etiology and risk factors for placenta previa: an overview and meta-analysis of observational studies. The journal of maternal-fetal & neonatal medicine Mar;13(3):175-90. doi: 10.1080/jmf.13.3.175.190.
Jansen CHJR, van Dijk CE, et al (2022) Risk of preterm birth for placenta previa or low-lying placenta and possible preventive interventions: A systematic review and meta-analysis. Front Endocrinol (Lausanne) Sep 2;13:921220. doi: 10.3389/fendo.2022.921220.
NHS Choices. Sex in pregnancy https://www.nhs.uk/conditions/pregnancy-and-baby/sex-in-pregnancy/ (Page last reviewed 16/03/2021 Next review due 16/03/2024)
Royal College of Obstetricians & Gynaecologists (2013) Air travel and pregnancy patient information leaflet | RCOG

