Treatment to prevent a premature birth
Why pregnancy should be prolonged
If you are at risk of giving birth early, your midwife or doctor may offer you treatment to try and stop this from happening. This will give your baby more time to develop in the womb and get ready for the outside world.
You may be offered treatment to prevent early labour if:
- you've given birth at less than 34 weeks pregnant before
- you've had a miscarriage after 14 weeks pregnant before
- your waters have broken before 37 weeks (PPROM), in this pregnancy or in previous pregnancies
- your cervix has been injured in the past, for example through surgery
- your cervix is shorter than expected (measured with an internal vagina scan).
If you are having more than 1 baby
The National Institute for Health and Care Excellence (NICE) recommends that all women carrying multiple babies should plan to give birth earlier than women carrying 1 baby. This helps to reduce the risk of complications.
This means that even if you don’t go into premature labour naturally, you will be advised to give birth before your due date.
You may be offered an induction (starting labour artificially) or a caesarean section. Exactly when this will be will depend on your circumstances. But if your pregnancy has been uncomplicated, this may be at:
- 37–38 weeks if you are carrying twins with their own placentas (dichorionic)
- 36–37 weeks if you are carrying twin babies that share a placenta (monochorionic)
- between 32 and 33+6 weeks if you are carrying twin babies that share a placenta and amniotic sac (monochorionic monoamniotic)
- 35 weeks if you are carrying triplets with their own placentas and amniotic sacs (trichorionic triamniotic), or 1 baby that has a separate placenta and 2 babies that share a placenta and all 3 babies have separate amniotic sacs (dichorionic triamniotic).
You’ll have an individual assessment to decide when to give birth if you:
- have had a complicated twin or triplet pregnancy
- are expecting triplets where all 3 babies share 1 placenta but each has its own amniotic sac (monochorionic triamniotic)
- a triplet pregnancy where any babies share an amniotic sac (dichorionic diamniotic monochorionic diamniotic or monochorionic monoamniotic).
Unless labour starts on its own, when you give birth is ultimately up to you. Your doctors will talk to you about the risks of continuing with the pregnancy beyond the recommended time. If you still don’t want to give birth at the recommended time, you’ll be offered weekly appointments with your specialist doctor. They will monitor your babies closely.
If you are at higher risk of premature labour starting on its own, you may still be offered treatments to prevent your babies from being born too early. These include progesterone, a cervical stitch or an arabin pessary. But these treatments may be less effective than in women carrying more than 1 baby, so they are not routinely offered to women carrying multiple babies. Bed rest is also not routinely advised.
You may be offered a medication called corticosteroids during your pregnancy to help your baby’s lungs develop more quickly. This can reduce the risk of complications associated with giving birth prematurely.
You will also be monitored with frequent scans for signs of twin-to-twin transfusion syndrome (TTTS), which can cause premature birth.
Find out more about giving birth to multiple babies.
Will I have a choice about what treatment I have?
It is really important that you are involved in every decision about your care and treatment. How you are treated is ultimately up to you, so your healthcare team should talk to you about what options are available and what the advantages and disadvantages are for each. Don’t be afraid to ask any questions that will help you help make an informed decision.
If you decide to go ahead with treatment, you will likely be asked to sign a consent form that states that you agree to have the treatment and you understand what it involves.
Monitoring – also known as the ‘wait and see’ approach
Your healthcare team may arrange for you to have transvaginal ultrasound scans to measure your cervix. If your cervix is found to be short (less than 25 mm long), you may be offered:
- a cervical stitch
- a hormonal treatment with progesterone
- a combination of the two treatments above
- close monitoring by your healthcare team.
Progesterone
Progesterone is a hormone that can help prevent contractions and help a pregnancy continue to full term. If your healthcare professional thinks you should take it, NICE recommends that women should be offered this from between 16 and 24 weeks of pregnancy and until you are at least 34 weeks pregnant. This will be given to you as a small tablet that you put into your vagina or bottom.
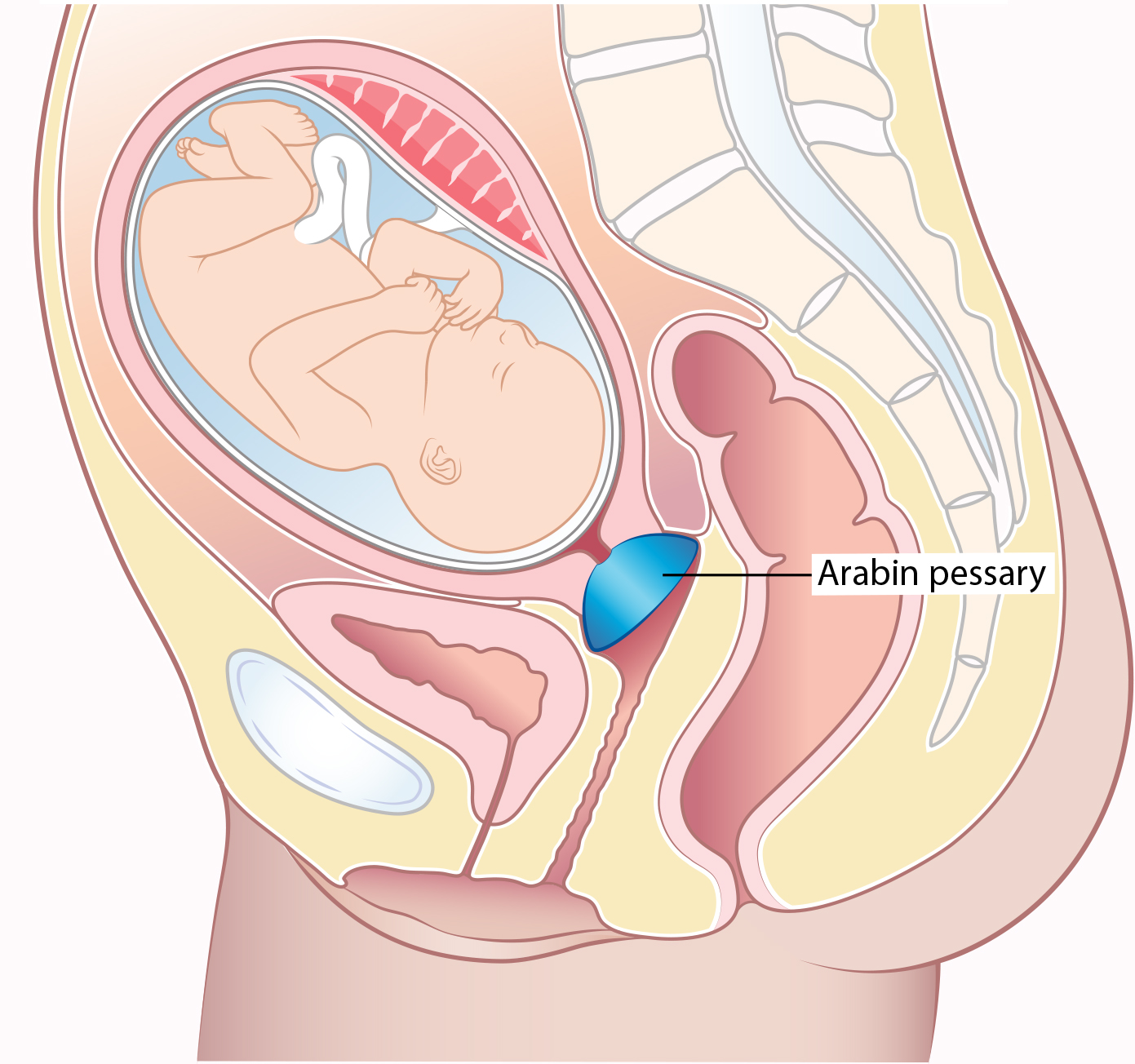
Arabin Pessary
The Arabin Pessary is a soft silicon ring that is inserted into the vagina by your doctor and moved into place so that the cervix sits inside it.
It is not used in all hospitals because there isn’t enough evidence that they work. Tommy’s Edinburgh Research Centre is looking at whether it can stop premature birth in women who are pregnant with more than 1 baby. Tommy’s London Research Centre is looking to see whether it works as well as a stitch or progesterone in women with single pregnancies.
You can ask your doctor or midwife for more information about the Arabin Pessary.
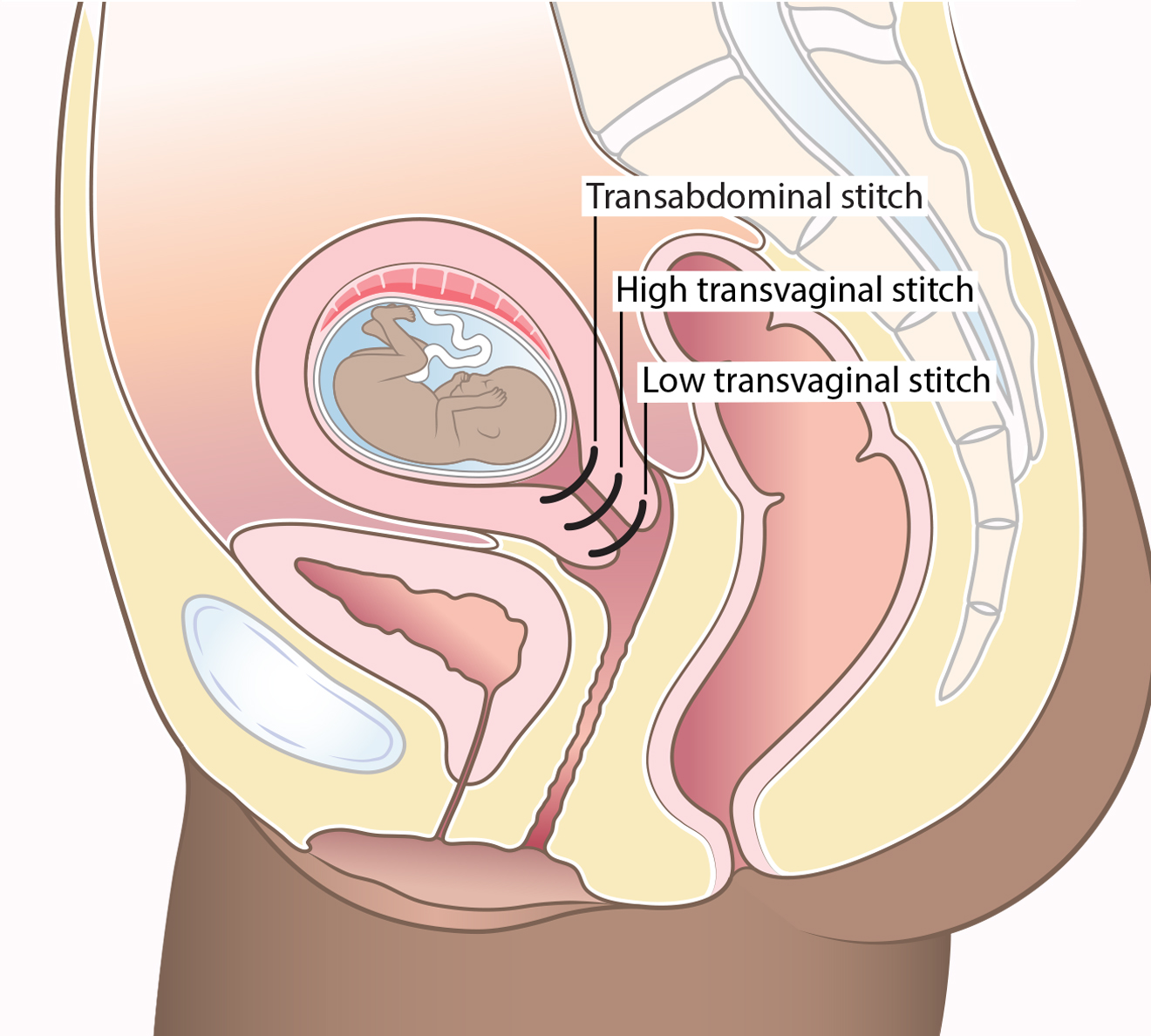
Having a cervical stitch
A cervical stitch is an operation where a stitch is placed around the cervix (neck of the womb). This may help to keep the cervix closed and reduce the risk of premature birth.
A cervical stitch is either put in vaginally (transvaginal) or through the abdomen (transabdominal). A transvaginal stitch is more common.
Is there any reason I couldn’t have a cervical stitch?
Sometimes you may be advised not to have a cervical stitch because it would be bad for your health or may not help prevent premature birth. This may happen if you:
- have any signs of infection
- are having vaginal bleeding
- are having contractions
- your waters have already broken (PPROM).
Are there any risks from having a cervical stitch?
Unfortunately, there are no guarantees that a cervical stitch will work, so you may still experience a late miscarriage or premature birth.
The risks of surgery are rare but include:
- bleeding
- infection
- injury to the bladder
- injury to the cervix
- your waters breaking early.
Having a cervical stitch is not always possible. For example, if your cervix is already too short or too far open. A vaginal cervical stitch does not increase your chances of needing an induction or a caesarean section.
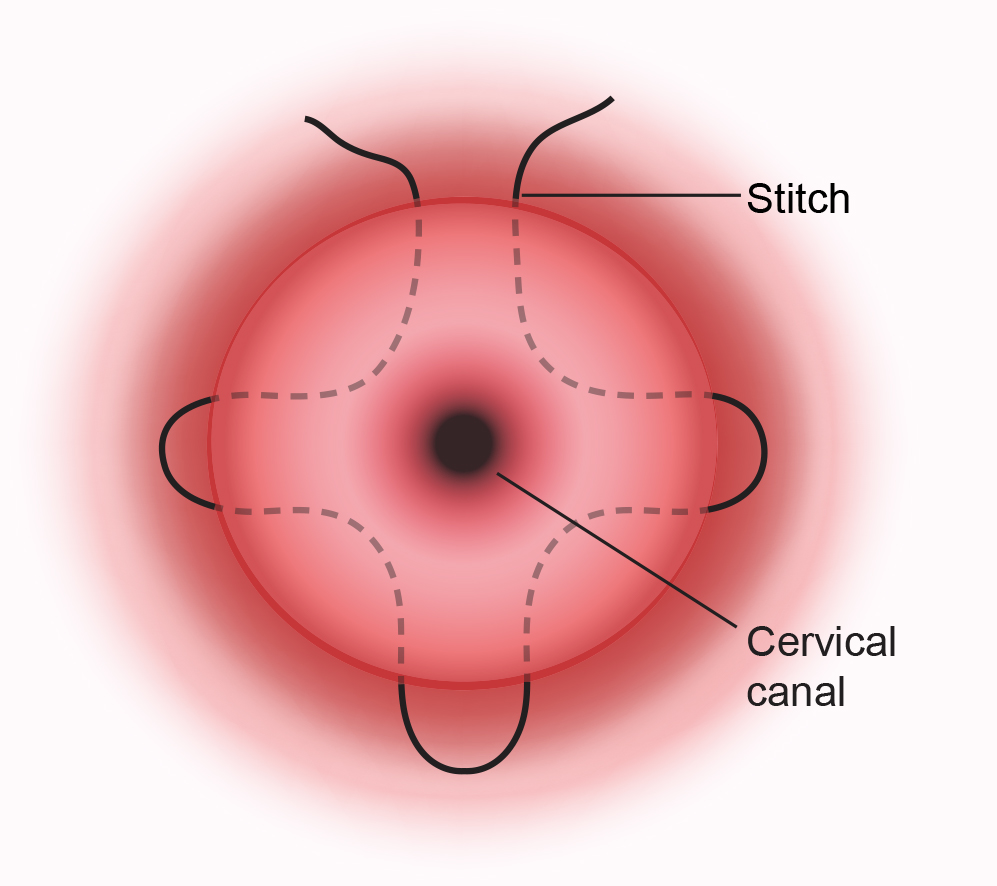
How is a transvaginal cervical stitch put in?
A vaginal cervical stitch is performed in an operating theatre in hospital. You’ll be given an anaesthetic that will make you numb from the waist down or that will make you sleep. Your healthcare professional will talk to you about which option is best.
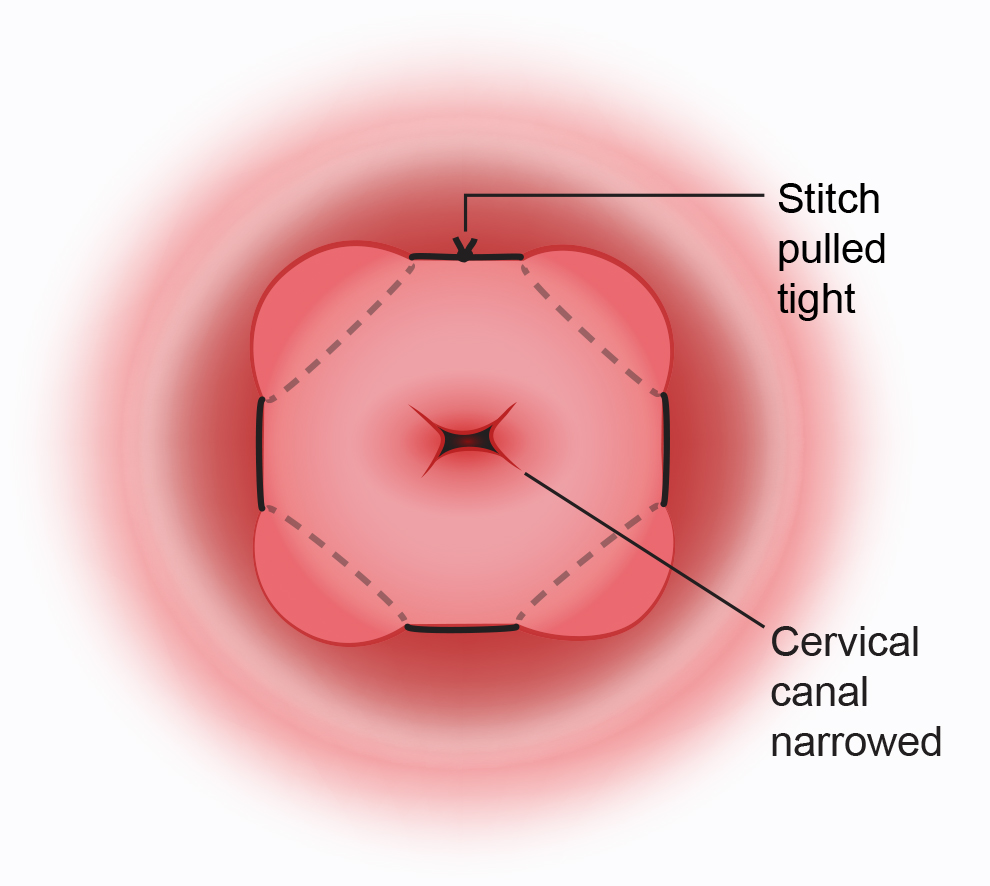
The surgeon will insert a speculum into your vagina, hold the cervix and put a stitch around it. The stitch is then tightened and tied, helping to keep the cervix closed. The operation usually takes less than an hour and you’ll be offered medication to ease any discomfort after the surgery.
There are 2 different types of vaginal stitch:
- low vaginal stitch (sometimes called a McDonald Cerclage)
- high vaginal stitch (sometimes called a Shirodkarstitchor TVCIC – Transvaginal cervicoisthmic cerclage).
Which type of stitch is used will depend on your personal situation and your healthcare professional. They should talk to you about this before the procedure.
When is a transvaginal cervical stitch put in?
A vaginal cervical stitch is usually done between 12 and 24 weeks of pregnancy. Rarely, it is done at an earlier or later stage.
How will I feel after having a transvaginal cervical stitch?
You may have some vaginal bleeding or brownish discharge for a day or 2. Once you recover, you can continue as normal for the rest of your pregnancy. You can have sex when and if you feel comfortable (unless you have been advised not to).
You should contact your healthcare team if you experience any of the following:
- contractions or cramping abdominal pain
- continued or heavy vaginal bleeding
- your waters breaking
- smelly or green vaginal discharge.
When is the transvaginal cervical stitch removed?
Your stitch will be taken out in hospital at around 36–37 weeks of pregnancy (unless you go into labour before then). A speculum is inserted into your vagina and the stitch is cut and removed.
This usually takes just a few minutes. You may experience some discomfort, but most women don’t need anaesthetic to numb the area.
You may notice some blood staining or vaginal spotting afterwards. This should settle within 24 hours, but you may have a brown discharge for longer. Tell your healthcare professional if you have any concerns.
Can I have a vaginal delivery after the transvaginal cervical stitch is removed?
Yes. Very rarely, scar tissue can form around the stitch, which prevents the cervix from dilating (opening) enough during labour. This makes a vaginal delivery more difficult. However, less than 3% of women need to have a caesarean section because of cervical scarring.
What if I go into labour when the stitch is in place?
If you go into labour with the cervical stitch still in place, you should contact your maternity unit straight away. It is important to have the stitch removed to prevent damage to your cervix.
If your waters break early but you are not in labour, the stitch will usually be removed because of the increased risk of infection. Your healthcare professional should talk to you about when this should happen.
What is a transabdominal stitch?
A transabdominal stitch is a cervical stitch that is put in through the abdomen. Your doctor may offer you transabdominal stitch if:
- you have had a transvaginal stitch before and it didn’t prevent a preterm birth
- you have a high risk of very early delivery and the shape of your cervix makes a transvaginal stitch impossible.
How is a transabdominal stitch put in?
The doctor will need to make a cut in your abdomen (stomach). You’ll be given an anaesthetic that will make you numb from the waist down or that will make you sleep. Your healthcare professional will talk to you about which option is best. You shouldn’t feel any pain, but there is pain relief available.
When is a transabdominal stitch put in?
You can have a transabdominal stitch before getting pregnant or in early pregnancy (before 14 weeks).
Does a transabdominal stitch always work?
There is no guarantee that a transabdominal stitch will work. But you will have a very good chance (over 90%) of giving birth when your baby is full term.
Can I have a vaginal birth after a transabdominal stitch?
No. You will need a caesarean section to deliver your baby when you are around 37–39 weeks pregnant. This is because the stitch will prevent the cervix from opening and labour could cause damage.
When is the transvaginal cervical stitch removed?
It is safe to leave this stitch inside your womb, so you will not need to have it removed. This may be helpful if you decide to have another baby.
You can request to have the stitch removed during your caesarean section, but it isn’t always possible.
What is a rescue stitch?
You may be offered a cervical stitch as an emergency procedure if your cervix has already opened and you are between 16 and 27 weeks pregnant. This can help prolong pregnancy. This is called a rescue stitch. This won’t be suitable if you:
- have signs of an infection
- have vaginal bleeding
- are having contractions.
This procedure carries risks and doesn’t always work. Your healthcare team will talk to you about the risks and benefits of this procedure.
What happens if the cervical stitch doesn’t work?
If the team at the hospital think you are going into labour with a cervical stitch, they will likely examine you and perform some tests to find out if you are in early labour.
If you have had a transvaginal cervical stitch, you will need to have it removed before your baby is born. This is because there is a risk of it tearing if it is still in place while you are having contractions.
If you had a transabdominal stitch, you’ll be advised to have a caesarean section.
Will I be advised to go on bed rest for premature birth?
There isn’t any research that proves that bed rest helps to prevent premature birth. But your midwife or doctor may offer this as a treatment. If so, they should discuss the pros and cons with you.
What are the warning signs of premature birth?
Pregnancy for women at high-risk of premature birth can be a very anxious time. If you are worried about any signs or symptoms, should contact your midwife or hospital immediately. Here are some possible signs of premature labour that you can look out for:
- regular contractions or tightenings
- period-type pains
- a "show" – when the plug of mucus that has sealed the cervix during pregnancy comes away and out of the vagina
- a gush or trickle of fluid from your vagina – this could be your waters breaking early (PPROM)
- backache that's not usual for you.
Tell your midwife or hospital staff immediately if:
- you are bleeding
- your baby is moving less than usual
- your waters have broken and they are smelly or coloured.
Find out more about the signs of early labour.
NICE (2019). Twin and triplet pregnancy. National Institute for health and care excellence https://www.nice.org.uk/guidance/ng137
Royal College of Obstetricians & Gynaecologists (2018) Cervical stitch. https://www.rcog.org.uk/en/patients/patient-leaflets/cervical-stitch/
NICE (2015). Preterm labour and birth. National Institute for health and care excellence https://www.nice.org.uk/guidance/ng25
Guy’s and St Thomas’ NHS Foundation Trust. Transvaginal cervical cerclage. https://www.guysandstthomas.nhs.uk/resources/patient-information/maternity/transvaginal-cervical-cerclage.pdf (Published January 2019 Review date January 2022)
Guy’s and St Thomas’ NHS Foundation Trust. Transabdonminal cervical cerclage. https://www.guysandstthomas.nhs.uk/resources/patient-information/maternity/transabdominal-cervical-circlage.pdf (Published January 2019 Review date January 2022)
Sosa CG et al. Cochrane Database of Systematic Reviews (2015) Bed rest in singleton pregnancies for preventing preterm birth. Cochrane Database of Systematic Reviews 2015, Issue 3. Art. No.: CD003581. DOI: 10.1002/14651858.CD003581.pub3.
NHS Choices. Premature labour and birth. https://www.nhs.uk/conditions/pregnancy-and-baby/premature-early-labour/ (page last reviewed 4 November 2019 Next review due 4 November 2022)
NHS Choices. Signs that labour has begun. https://www.nhs.uk/conditions/pregnancy-and-baby/labour-signs-what-happens/ (30 November 2020 Next update due: 9 November 2023)

