Perineal tears
What is a perineal tear?
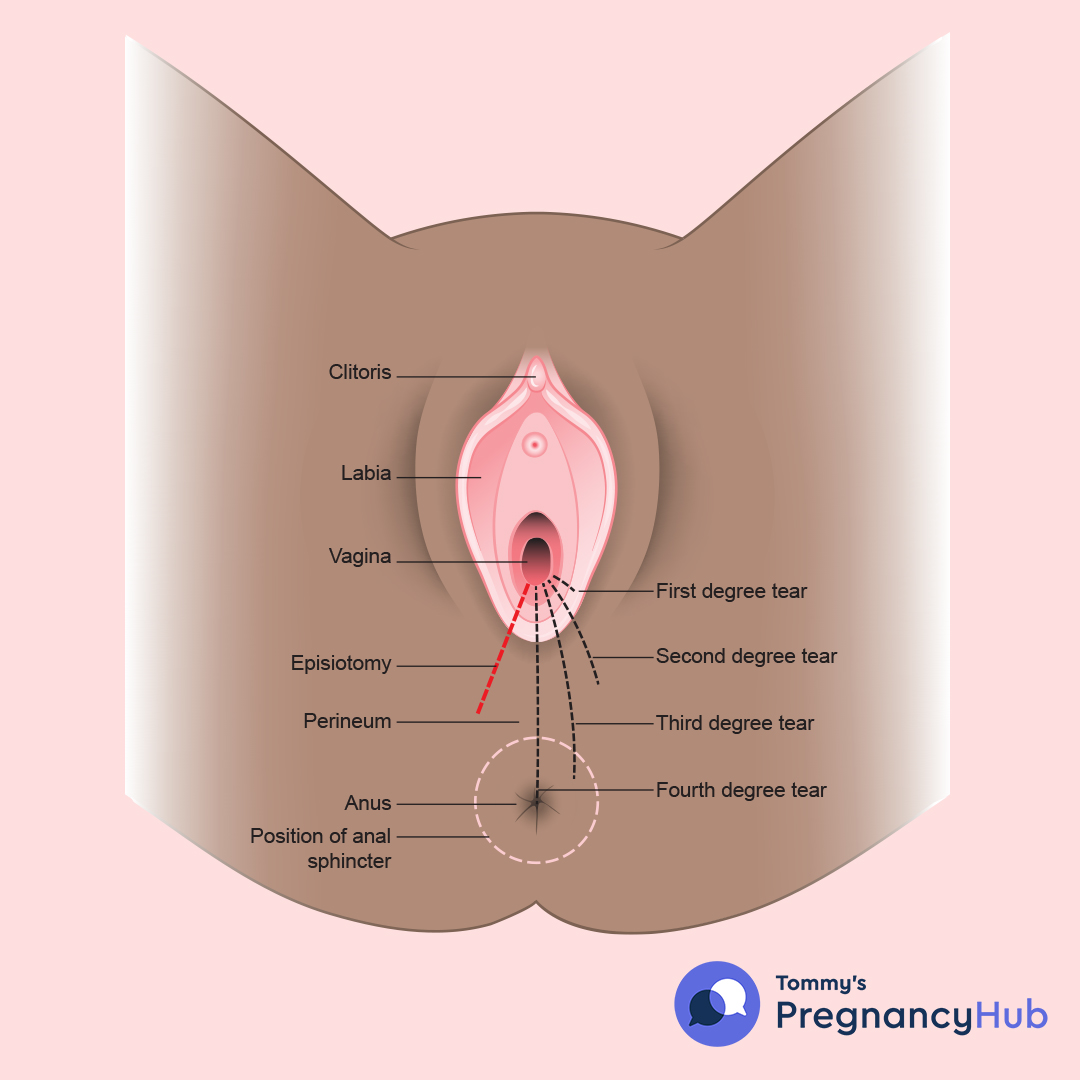
Your perineum is the bit between your vaginal opening and anus. Tears tend to happen as the vagina and perineum stretch during your baby’s birth.
Tears can also happen inside the vagina or other parts of the vulva, such as the labia (the inner and outer lips of the vagina).
Some women and birthing people call their tears ‘birth injuries’. They don’t feel ‘tear’ really conveys what’s happened to them. We will use the medical term perineal tears here.
Are perineal tears common?
Up to 9 in 10 people who have a vaginal birth for the first time will have some sort of tear, graze or episiotomy (when a doctor or midwife makes a cut between the vagina and anus during childbirth).
For most people, these tears are minor and heal quickly.
What are the types of perineal tear?
- First-degree tears are small and only affect the skin. They tend to heal quickly and without treatment. They are not likely to cause long-term problems, but they can be very sore.
- Second-degree tears affect the muscle of the perineum and the skin. They may well require stitches. Second-degree tears are not likely to cause long-term problems, but can be very sore.
- Third-degree tears extend into the muscle that controls the anus (the anal sphincter).
- Fourth-degree tears extend further into the lining of the anus or rectum.
Around 6 out of 100 people who have a vaginal birth for the first time will have a third-degree or fourth-degree tear. Less than 2 in 100 people who have had a vaginal birth before will have a third-degree or fourth-degree tear.
These deeper tears will most likely need to be repaired through surgery.
Rectal buttonhole
A rectal buttonhole is a rare injury that occurs when the anal sphincter does not tear, but there is a hole between the back passage and the vagina.
This means that wind and faeces may be passed through the vagina instead of through the anus.
What makes a perineal tear more likely?
There’s often no clear reason why third-degree and fourth-degree tears happen. But they are more likely if:
- this is your first vaginal birth
- your baby is over 4kg (9lb)
- you have a long second stage of labour (also known as the pushing stage)
- your baby’s shoulder gets stuck (known as shoulder dystocia)
- you are of Asian ethnicity
- your midwife or doctor needs to use forceps or a ventouse to deliver your baby (assisted birth)
- your baby is occipito-posterior (facing with their back to your back) or breech
- your labour is very quick (known as precipitous birth).
Find out more about getting your baby into the best birth position.
How can I avoid a perineal tear?
There are some things that can reduce your risk of tearing during childbirth. You can talk to your midwife about these at any time during your pregnancy. You can also find out more during antenatal classes.
Perineal massage
Massaging the perineum in the last few weeks of pregnancy can reduce the chances of tearing during birth. The Royal College of Gynaecologists and Obstetricians has a guide on how to massage your perineum.
Birth position
Kneeling down, being on all fours or lying on your side during labour may reduce the risk of tearing or reduce how much you tear. Find out more about positions during labour.
How your midwife can help
Your midwife will also help you avoid a tear during labour. When the midwife can see your baby’s head, they will ask you to stop pushing and to pant or puff a couple of quick short breaths, blowing out of your mouth.
This will help your baby’s head emerge slowly and gently, giving the skin and perineum muscles time to stretch without tearing.
Your midwife or doctor may also gently place a warm compress on the perineum as the baby’s head comes out. This may not stop tearing but may reduce how much you tear. You can ask your midwife about this.
Where you give birth
It’s also thought that giving birth at home or in a midwife-led unit may help reduce the risk of tearing. This may be because some people feel more relaxed in these places.
It’s normal to feel worried or confused about where the best place for you to give birth is, but your midwife will be there to help explain your options. They can talk to you about the pros and cons of each choice, and help you make the right choice for you. Find out more about where you can give birth.
Some research has suggested that having a water birth can help you avoid tearing. But there is not enough evidence to prove this is true.
How does a tear differ from an episiotomy?
A tear happens on its own (spontaneously) as the baby stretches the vagina during birth. An episiotomy is a cut made by a midwife or doctor into the perineum and vaginal wall to make more space for your baby to be born.
A doctor or midwife will most likely do an episiotomy if you are having an assisted vaginal birth (where instruments are used to help deliver your baby). Episiotomies are only done with your agreement (consent).
You may also have an episiotomy either to prevent a more major tear or to speed up delivery because your midwife is concerned about the baby.
This can only be done if your doctor or midwife can see the baby’s head coming out of the birth canal (crowning).
Sometimes, an episiotomy may extend and become a deeper tear. If you have had an episiotomy, you will need stitches to repair it.
Will I feel a tear happening during childbirth?
During the second stage of labour (also known as the pushing stage), your body will guide you on how and where to push.
As the baby’s head meets your perineum (the bit between your vagina and anus), the urge to push becomes stronger, and so does the feeling that you want to open your bowels.
Often, your body will push or bear down without you even knowing it. It is a reflex and is almost impossible to stop, so it is best to go with it.
Due to the amount of pressure caused by your baby’s head on your perineum, it not likely that you will feel any tearing.
But each birth is different, and some people may find that they feel a lot of stinging, especially as the head is crowning (when baby’s head can be seen coming out of the birth canal).
Your midwife will guide you through this time to slow the crowning of the baby’s head and allow the muscles to stretch slowly as the head is delivered.
How will I know if I have torn?
Your midwife or doctor will check you over right after you have your baby. They will record your temperature, check your pulse and your blood pressure.
They will also need to check your genital area to see if it has torn and whether you need stitches. This may include a rectal examination, where the midwife or doctor uses their finger to check for any problems inside your bottom (rectum).
Your midwife or doctor should explain to you what they are going to do. They will ask you to move or help you get into a comfy position so they can see clearly.
You may be offered some gas and air while they do an internal check for vaginal tearing.
Can I hold my baby while I’m being examined?
Yes, you can usually hold your baby while you are being examined. Your healthcare team should encourage you to have skin-to-skin contact with your baby right after the birth, unless there is a medical reason why not.
Skin-to-skin means having your baby on you, their naked skin next to yours, with a blanket over both of you for warmth (you can put it in your birth plan). Find out more about the benefits of skin-to-skin.
You may not be able to hold your baby if you have bleeding that needs urgent attention. If you can’t hold your baby, your birthing partner will be the next best person if you have one.
If I need stitches, will these be done straight away?
Unless your midwife or doctor thinks you need to be moved elsewhere (see below), any stitches you need will be done straight away. This will reduce any chance of infection or blood loss.
Will I have to be moved if I have torn?
Your midwife or doctor can usually assess the genital area and do any stitches where you have given birth. If you have not given birth on a labour ward in a maternity unit, you may need to be moved there if:
- your healthcare professional needs support with their assessment from a more senior midwife or doctor
- your repair needs more surgical expertise.
If you have a third-degree, fourth-degree or rectal buttonhole tear, you will be transferred to theatre as soon as possible after your baby is born.
Will the stitches hurt?
If you’ve had a small tear, you’ll be given a local anaesthetic to numb the area so that you won’t feel any pain from the stitches.
You may need to put your legs into stirrups while the stitching is carried out. If the pain relief doesn't seem to be working at any stage, you should let the midwife or doctor know. They can give you more if needed.
You may be given a regional anaesthetic (designed to numb your genital area) or spinal anaesthetic if you have significant trauma and you need to go to an operating theatre at hospital.
If you had an epidural for labour, that can usually be topped up so you have pain relief for the procedure, instead of having another type of anaesthetic.
After your stitches are in place, you may be offered a small rectal suppository (a tablet that goes into your bottom). This may help calm any inflammation and pain.
You should be told about the extent of the trauma and how to look after yourself at home.
How long will it take for the stitches to heal?
It is normal to feel pain or soreness for 2 to 3 weeks after having any tear. The stitches may also irritate and it may sting when you wee. They may feel a little itchy, but this often means they are healing.
The skin part of the wound is likely to heal within a few weeks of giving birth. If you have a third- or fourth-degree tear this may take longer to heal. You may be given antibiotics to stop infection.
Most tears are repaired with stitches that dissolve, which means they soften and fall out on their own. You normally won’t have to go back to hospital to have your stitches removed.
How do I look after my stitches when I go home?
Keeping the area clean
Good hygiene helps reduce the risk of infection. To keep the area clean:
- Have a shower or bath every day and use only water on the area. You can use the shower head to gently wash the wound. Do not rub soap into it.
- Wash your perineum and the area around it after every trip to the toilet. Make sure the wound is dry by patting with a clean dry towel.
- Change your maternity pads often, to reduce the risk of infection. (You will have some bleeding after birth).
Easing any pain or discomfort
To help with any pain:
- Take paracetamol, which can help with stinging, or ibuprofen, which can help with swelling. Both are safe to take if you’re breastfeeding, but make sure you read the labels. Avoid aspirin as it can be passed to your baby if you breastfeed or chestfeed. You can also ask your doctor or midwife if you are unsure what tablets to take.
- Put an ice or cool pack on the region for about 10 minutes at a time. Wrap this in a clean flannel or towel to avoid ice-burn, which can be painful. Your midwife may also suggest using a maternity pad that has been kept in the fridge or freezer.
- Take a warm bath.
- Sit on a rubber ring (for no more than half an hour at a time as this can restrict circulation).
- Change your position often. You could try standing up for a bit, then sitting down or lying on your side.
- Use a small jug to pour warm water over your perineum during and after weeing, which can help with the stinging.
- Try to eat a healthy balanced diet and stay hydrated to avoid painful constipation. If you are still constipated, see a pharmacist or GP, who may be able to give you something to make your stools softer.
Some pharmacies and chemists sell creams or sprays that contain local anaesthetic. But these can be costly, and there is no real proof that they work.
Helping the area to heal
To help healing:
- Avoid using a hairdryer on it (even on a cool setting) as this can damage the tissue. Dust and hair can also blow off the hairdryer and get stuck in the wound, causing infection. Use a clean towel to pat the area dry instead.
- Wear breathable fabrics, such as cotton. Disposable briefs with loose clothing can also help.
- Expose the wound to fresh air by taking off your underwear and lying on a towel on your bed for around 10 minutes, once or twice a day.
- Do your pelvic floor exercises. This helps increase the blood flow to the area and speed up the healing process. Doing pelvic floor exercises will also help strengthen the muscles around the vagina and the anus, which should help improve any issues with controlling your bowels. Your midwife can explain how to do these if you are unsure.
- Avoid smoking as this can affect how well the wound heals.
- Avoid heavy lifting or intense exercise for 4-6 weeks after childbirth.
- Do not use any cream, lotions or sprays that contain steroids. These can slow down the healing process.
Tell your healthcare professional if you have any concerns
Tell your midwife, health visitor or GP if:
- your stitches become painful
- your stitches become smelly
- your wound does not heal
- you have been diagnosed with a first- or second-degree tear, but you are having problems controlling your bowels, for example if you struggle to make it to the toilet or control wind
- you pass poo through your vagina
- you have a fever (a sign of infection)
- you have any other concerns.
“My son arrived in a bit of a rush as he was becoming distressed and I needed a forceps delivery. The epidural worked really well for my pain relief and the stitches afterwards. At home, I took regular paracetamol and ibuprofen, but after a few days noticed that my stitches were pulling apart and the pain was getting worse.
“I showed my midwife, who referred me back to the hospital, where the doctor advised that I should take a week of antibiotics to prevent infection and that healing would take place more slowly. I had to really remind myself to do those pelvic floor exercises every time my son had a feed. After about 2 months, everything healed. Talking to other mums now, I realise a lot of them have had a similar experience.”
Seema
What happens when I have a poo?
Your stitches shouldn’t be affected when you do a poo. Try to avoid constipation by eating a healthy, balanced diet and drinking at least 2 litres of water a day.
If you have had a third-degree or fourth-degree tear, you’ll be given some laxatives (a medicine that helps loosen your poo) so you don’t need to push too hard when you poo. These may work so well that you may not get to the toilet in time. This should improve after a couple of days.
The following tips may also help you poo:
- Put your feet on a footstool to raise your knees above your hips while you sit on the toilet.
- Take deep breaths to avoid straining.
- Gently push down from your bottom rather than holding your breath.
- Take your time and don’t rush.
- Don’t delay if you need to go to the toilet.
- Do your pelvic floor exercises.
When wiping your bottom, make sure you wipe gently from front to back. This helps to protect your wound from bacteria.
What is the likelihood of a tear causing complications like incontinence?
A first-degree or second-degree tear is not likely to cause incontinence (when you poo or wee without meaning to).
1 in 3 women and people who give birth have urinary incontinence (weeing without meaning to) after having a baby, whether they had a tear or not. It may help to:
- do your pelvic floor exercises
- stop smoking
- avoid high-impact exercise (such as jogging)
- avoid heavy lifting (such as older children or shopping bags)
- treat constipation quickly
- cut down on caffeine
- avoid alcohol
- avoid spicy or acidic foods
- drink 6 to 8 glasses of water a day.
In time, if you are overweight, it may also help to try and lose some weight slowly. This is because being overweight can weaken pelvic floor muscles. Losing excess weight is easier said than done after having a baby and there is no rush. Your body needs time to recover.
If you had a more complicated delivery or a caesarean, your recovery time will be longer, too. There’s no need to start doing high impact exercise or go on a diet.
Just try to eat a healthy balanced diet, drink plenty of water and do some light movement, such as walking, until you are ready to do more).
Find out more about your body after birth.
Faecal incontinence
Anal or faecal incontinence is when you have problems controlling your bowels. Symptoms include a sudden uncontrollable urge to poo, passing wind uncontrollably or leaking poo.
Most people who have a third-degree or fourth-degree tear have no lasting complications and heal fully. Some people may have problems with faecal incontinence. For most, this issue gets better. But it may be an ongoing complication for a small number of people.
Do not be afraid or embarrassed about talking to a healthcare professional about it. There are things they can do to help. You may need extra care, such as surgery, or physiotherapy to help strengthen your sphincter muscles.
Should I have a follow-up appointment after having a tear?
Many hospitals will offer a check-up if you have had a third-degree or fourth-degree tear. You may also be seen by a specialist women’s health physiotherapist.
Your GP surgery should offer you a postnatal check 6 to 8 weeks after your baby’s birth to make sure you are feeling well and are recovering as you should be.
They may offer to look at how your stitches are healing, or you can ask them to check.
Your health visitor can also check how you are healing. Don’t feel you have to wait for this appointment with the GP, though. Call your midwife, health visitor or GP if you have any concerns about your stitches.
Will I need to go back and have the stitches taken out?
No. The stitches take about a month to dissolve on their own.
How much can I move if I’ve had stitches?
Everyone is different, so listen to your body and take things slowly. If you’ve had a more severe tear, it’s best to avoid strain or pressure on the area and avoid intense exercise or heavy lifting for around 4-6 weeks.
It can be hard to look after a baby when you are recovering from giving birth and you need to take time to rest and heal. Take any offer of help you get from a partner, family or friends so you can focus on your healing.
Is it possible for the stitches to break?
It is rare for the stitches to come undone. But sometimes an infection, or pressure on the stitches from bleeding underneath, can cause the stitches to break and leave an open wound. This is called perineal wound dehiscence or breakdown.
Wound breakdown can cause pain, new bleeding or pus-like discharge. You may also begin to feel unwell, especially if you have an infection. Sometimes people notice some stitch material coming away soon after they have had their baby, or can see for themselves that the wound has opened.
Call your midwife, health visitor or GP if you have any concerns about your stitches. If your stitches have broken, you will likely need further treatments. Your healthcare professional will be able to advise what to expect.
When can I have sex again?
From a physical point of view, you can start having sex again once your stitches are healed and bleeding has stopped. But it’s also important to think about whether you are emotionally ready to start having sex again.
Find out more about sex after pregnancy.
When can I exercise again?
It's good to wait until after your 6-week postnatal check before you start any high-impact workouts, such as running. If you had a more complicated delivery or a caesarean, your recovery time will be longer.
Talk to your midwife, health visitor or GP before starting intense exercise again.
If you’ve had a third-degree or fourth-degree tear, it may help to:
- mix resting with gentle walks and light activity
- try to avoid lifting anything that’s heavier than your baby for the first 6 weeks
- let someone else lift the buggy, car seat and any other children you have, if that’s an option
- keep doing your pelvic floor and postnatal exercises.
Will I tear again if I have another baby?
Many people go on to have a straightforward vaginal birth after a severe tear.
Some people think about having a planned caesarean section next time. You’ll be able to talk about how you feel and what your options are at your follow-up appointment or early in your next pregnancy.
I feel traumatised by my birth experience. How do I cope with this?
Tearing during labour, especially if you have a third-degree or fourth-degree tear, can be a source of great distress. Your birth partner (if you have one) may also be traumatised. Find out more about recovering after a traumatic birth.
It’s normal to have upsetting thoughts right after a traumatic event. For most people, these thoughts improve over time on their own.
However, some people may develop post-traumatic stress disorder (PTSD). PTSD is an anxiety disorder caused by very distressing events.
People with PTSD may have persistent flashbacks of the event, and can feelings irritable, guilty or lonely. This may lead to a fear of childbirth (tokophobia) in the next pregnancy.
PTSD can start soon after an event or it can happen weeks, months or even years later. You should see your GP if you are still experiencing problems 4 weeks after giving birth, or if your symptoms are getting in the way of your daily life.
It can be very hard to come to terms with trauma, but PTSD can be treated. The key thing is to try and confront your feelings with help from healthcare professionals.
Talk to your GP or midwife if you are struggling after a traumatic birth. They will be able to help you get the right support.
Find out more about post-traumatic stress disorder.
More support and information
The Masic Foundation supports people who have incontinence following an injury during childbirth.
The Birth Trauma Association (BTA) supports people who suffer birth trauma – a shorthand term for post-traumatic stress disorder (PTSD) after birth.
Edozien LC., Gurol-Urganci, I. et al (2014) ‘Impact of third- and fourth-degree perineal tears at first birth on subsequent pregnancy outcomes: a cohort study’. BJOG. 121(13):1695-703. doi: 10.1111/1471-0528.12886.
NHS Inform (2023) How your baby lies in the womb. Available at: https://www.nhsinform.scot/ready-steady-baby/labour-and-birth/getting-ready-for-the-birth/how-your-baby-lies-in-the-womb (Accessed February 2024) (Page last reviewed 19/12/2023)
Lindgren, H. E., Brink, Å., & Klinberg-Allvin, M. (2011). ‘Fear causes tears - perineal injuries in home birth settings. A Swedish interview study’. BMC pregnancy and childbirth, 11, 6. https://doi.org/10.1186/1471-2393-11-6
NHS Choices (2023). 10 ways to stop leaks. Available at: https://www.nhs.uk/conditions/urinary-incontinence/10-ways-to-stop-leaks/ (Accessed February 2024) (Page last reviewed 15/06/2023, Next review due 15/06/2026)
Royal College of Obstetricians & Gynaecologists (nd.) Perineal tears and episiotomies in childbirth. Available at: https://www.rcog.org.uk/en/patients/tears (Accessed February 2024)
Milton Keynes University Hospital NHS Foundation Trust (2018) Care of your perineum after the birth of your baby. Available at: https://www.mkuh.nhs.uk/wp-content/uploads/2021/03/Care-of-your-perineum-after-the-birth-of-your-baby-PIL.pdf (Accessed February 2024) (Page last reviewed 08/2018, Next review due 04/2026)
NHS Choices (2023) Episiotomy and perineal tears. Available at: https://www.nhs.uk/conditions/pregnancy-and-baby/episiotomy/ (Accessed February 2024) (Page last reviewed 09/06/2023 Next review due 09/06/2026)
NHS Choices (2022) Keeping fit and healthy with a baby. Available at: https://www.nhs.uk/conditions/pregnancy-and-baby/keeping-fit-and-healthy/ (Accessed February 2024) (Page last reviewed 06/12/2022 Next review due 06/12/2025)
NHS Choices (2022) Post-traumatic stress disorder (PTSD). Available at: https://www.nhs.uk/conditions/post-traumatic-stress-disorder-ptsd/ (Accessed February 2024) (Page last reviewed 13/05/2022 Next review due 13/05/2025)
NHS Choices (2022) Your 6-week postnatal check. Available at: https://www.nhs.uk/conditions/pregnancy-and-baby/postnatal-check/ (Accessed February 2024) (Page last reviewed 28/11/2022 Next review due 28/11/2025)
NICE (2023) Intrapartum care: NICE clinical guideline 235. Available at: https://www.nice.org.uk/guidance/ng235 (Accessed February 2024) (Page last reviewed 29/09/2023)
Royal College of Obstetricians & Gynaecologists (2015). The management of third- and fourth-degree perineal tears. (Accessed February 2024) (Page last reviewed 06/2015) Available at: https://www.rcog.org.uk/globalassets/documents/guidelines/gtg-29.pdf
Royal College of Obstetricians & Gynaecologists (nd.) Your pelvic floor. Available at: https://www.rcog.org.uk/en/patients/tears/pelvic-floor/ (Accessed February 2024)
Sheffield Teaching Hospitals NHS Foundation Trust (2022) Physiotherapy advice following a third or fourth degree tear. Available at: https://publicdocuments.sth.nhs.uk/pil3469.pdf (Accessed February 2024) (Page last reviewed 11/2022 Next review due 11/2025)
Macdonald, S., Johnson, G. (2017) Mayes’ Midwifery. Edinburgh: Baillir̈e Tindall Elsevier.
Thom, DH., Rortveit G. (2010) ‘Prevalence of postpartum urinary incontinence: a systematic review’. Acta Obstetricia et Gynecologica Scandanavica. 2010 Dec;89(12):1511-22. doi: 10.3109/00016349.2010.526188. Epub 2010 Nov 5. PMID: 21050146.

